Insights from our first Pacific advisory fono
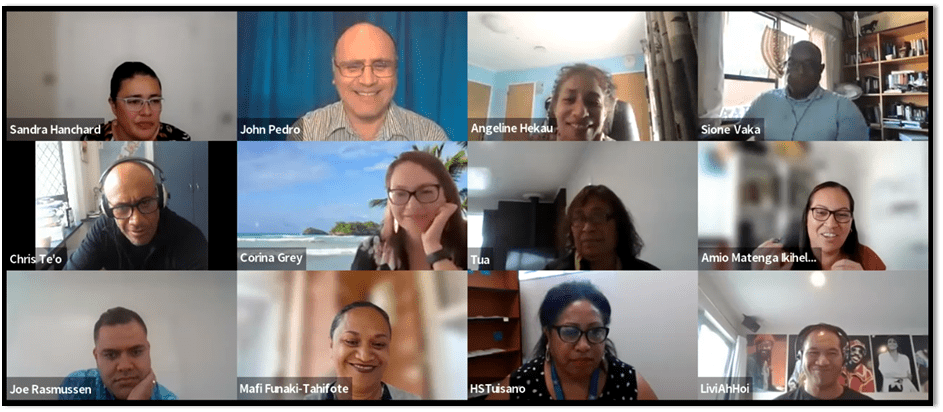
The Manawataki Fatu Fatu Heart Health Research Programme has established a Families and Pacific Advisory group to ensure that our research is authentically connected to the needs and wishes of Pacific families and communities. The advisory group comprises Pacific community leaders who will provide support and guidance on the direction of our research. Hosted in March 2022 over zoom, the purpose of our first talanoa was to make introductions and connections, to share an overview of the aims of Manawataki Fatu Fatu and receive some early feedback on our progress. It was inspiring to bring together a group of community leaders where we could share our aspirations for achieving optimal heart health outcomes for Pacific people.
Our Pacific advisory team consists of: Livi Ah Hoi, Mafi Funaki-Tahifote, Joe Glassie-Rasmussen, Angeline Hekau, Amio Ihikele, John Pedro, Christopher Te’o and Hana Tuisano
Manawataki Fatu Fatu is represented by: Corina Grey, Tua Taueetia-Su’a, Sione Vaka and Sandra Hanchard
These were some of the key themes that were brought up by the group:
Traditional healing practices and spirituality are interlinked for Pacific people
- In Pacific health we have our own healing models and medicinal practices (e.g. blends from leaves) for pain management and addressing illnesses.
- However, we may be reluctant to disclose traditional and/or religious practices with health professionals in biomedical contexts.
- Western medicine and traditional Pacific health practices can sit alongside each other. There is value in using our cultural forms of medicine: listening to the stories, sharing the different angles and moving forward together.
Balancing diet and medications are important for wellness
- What we eat and drink is top-of-mind for Pacific people when managing our health.
- More education is needed on the consumption of all types of fluids (e.g. kava) and impact on conditions such as heart failure (fluid retention) and diabetes (e.g. ‘noni drink’ and blood glucose control).
- Doctors are not always aware of what else is happening with their patient’s diet and the impact of medication. This is due to patients feeling that traditional practices are ‘taboo’ to discuss, language issues and doctors not asking.
- Reflections from the Niue community: Matua (elders) passed on wisdom that food is not an indulgence, and we should ‘eat for wellness’. This means ‘listening to our body’ and knowing limits. Yet, for others, medication can give people a license to ‘eat what they like’.
We need comprehensive and innovative approaches to education for heart health management
- Patients are given ‘cocktails of medication’, but little time is spent by the healthcare provider on what each pill does, potential side effects, why it’s needed, what it’s going to do, and the benefits e.g., “this medication will help you breathe easier, and you’ll have more energy.”
- Younger generations are more comfortable in questioning providers, but this is more difficult for elders when there are language barriers.
- Education could be given in different forms (e.g. videos, written) depending on people’s learning styles and preferences – media could be different for age and ethnic groups etc. Additional marketing efforts can increase awareness of verified and high quality information sources.
- More education is needed on recognising symptoms and when to seek help (e.g. example of Niue study where women not always using medications such as angina spray and using massage instead to relieve chest pain).
- We can explore innovative technologies for preventative approaches, such as AI/machine learning for predicting risk of having a heart attack. These tools should be offered in Pacific languages.
Sharing lived experiences and more considered engagement will shift attitudes to heart health
- We need to hear stories of heart health experiences from others in Pacific communities to strengthen messages of getting your heart health checked early and other important health advice.
- The first point of contact with the health system is crucial: A toolkit to support Pacific and non-Pacific clinicians on how to relate and communicate with patients will improve engagement. Simple gestures of taking the time to know and expressing an interest in patients will encourage reciprocal engagement with the health system.
- Greeting people in their preferred language can do wonders for engagement.
- It is confusing for patients and whānau to navigate the system – we need to have good advice and pathways for people to access good social and welfare supports (and to know their entitlements) after a heart event or diagnosis.
Next steps.. we need early buy in from all stakeholders
We need to involve all stakeholders, including community and providers in primary/secondary health, in the development of our Equity Roadmap. Each of us are responsible through our contributions. A key aim is to address deficits in what clinicians believe is needed or wanted by Pacific patients and whānau by grounding our research in the community and communicating these findings back to providers.
The Manawataki Fatu Fatu team would like to express their sincere gratitude to our Pacific advisory panel for sharing their wisdom and insights with us. We look forward to the next fono.
Recent Comments